Original Article
Ghazala Tabassum,
Imran Ghayoor, Riaz Ahmed
Pak J Ophthalmol 2013, Vol. 29 No.1
. . . . . . . . . . . . . . . .
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . . .. . .. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
. . . .
|
See end of
article for authors
affiliations …..……………………….. Correspondence
to: Ghazala Tabassum House # 106 Block-H, Karachi …..……………………….. |
Purpose: To evaluate the effectiveness of conventional
trabeculectomy in controlling intraocular pressure in patients with POAG in
our population. Material and Methods: This case control study was carried out
in department of ophthalmology, Liaquat National Hospital Karachi from 21st March 2005 to 20th
March 2006. 50 patients included in this study were diagnosed case of POAG,
who underwent conventional trabeculectomy. Mean follow up was one year.
Outcome measures were intraocular pressure and visual acuity. Results: The study included 50 patients with POAG who
undergone conventional trabeculectomy. Age range of patients was 41 – 74 with
the mean 56.8 years. Visual acuity showed no statistically significant
difference between pre and post-operative periods. Pre-op intra ocular
pressure was 20 – 55 mmHg and it was reduced to a mean of 5-22 mmHg post
operatively. The mean decline in IOP after surgery was 15.78 mmHg. Perimetry
and C/D ratio showed no significant change after surgery. Conclusion:
Results
show that in most of the cases visual acuity is maintained and IOP is
controlled in the short term period of one year. So conventional
trabeculectomy can be effective in controlling IOP in our population. |
Glaucoma
is the second leading cause of blindness worldwide1. Three
quarters of people with glaucoma have the open-angle variant, of whom 10% are
bilaterally blind2. Although it is generally a bilateral disease,
its severity may be asymmetrical in two eyes. It has an adult onset, open and
normal appearing angles on gonioscopy with the evidence of glaucomatous optic
nerve damage. This optic nerve damage may take the form of changes in the
appearance of the optic disc or nerve fiber layer or the presence of
abnormality in visual fields.3 Several factors have been implicated
as risk factors in the development of glaucomatous optic nerve damage such as
elevated intraocular pressure (IOP), myopia and changes in the appearance of
the optic nerve, family history of glaucoma, age, black race, diabetes mellitus
and cardiovascular diseases.4
Treatment
modalities of Glaucoma consist of topical and systemic medication, laser
treatment5 and conventional surgical procedures6.
Traditionally maximum tolerated medical therapy has been used before laser
trabeculoplasty or conventional surgery.
Trabeculectomy lowers IOP by
the creation of a new channel (guarded fistula) for aqueous outflow between the
anterior chamber and subtenon space. Performed early this filtering surgery
gives excellent IOP control with minimal complications7. We
conducted this study to document the effectiveness of conventional
trabeculectomy in controlling IOP in our population.
MATERIAL AND METHODS
This
study was carried out in the department of ophthalmology of Liaquat National
Hospital from 21st March 05 to 20th March 06. After informed consent, 50 patients (28 male and 22
female) were selected in the study. The age range of patients was 41 – 74 with
the mean 56.86. Inclusion criteria were patients with POAG undergoing
conventional trabeculectomy. Exclusion criteria were patients having secondary
glaucoma, primary / secondary angle closure glaucoma and history of prior
surgery. Complete biodata and detailed history were taken from all subjects
about his / her eye illness as well as systemic illnesses. Detailed ophthalmic
examination including visual acuity with and without pinhole, objective and
subjective refraction, papillary examination, color vision; adnexa, anterior
and posterior segment examination by Slitlamp, anterior chamber angle was
assessed with goniolens. Intraocular pressure was measured with Goldmann
application tonometer. 30–2 visual field analysis was performed with
computerized (Humphry) perimeter.
After
confirming as a case of POAG, patients were kept on list for trabeculectomy.
Patients who had IOP more then 40 mmHg were given pre op 20% mannitol 200 ml
I/V in 20 minutes.
Patients
were kept on regular follow up for one year. Follow up consists of six visits
postoperatively, done at 1st day, on 1st week 1st,
3rd, 6th and 12th months At each visit,
refraction, visual acuity best corrected visual activity, IOP, anterior chamber
depth and pupil reaction and bleb appearance. C/D ratio with +90D lens was
analyzed. Massage was done to reform the bleb where needed. Visual fields
analysis was performed with computerized perimetry (Humphery) in 6th
and 12th post operative months.
Statistical package for social
science (SPSS) 10.0 version was used to analyze data. Relevant descriptive
frequency and percentage was computed for qualitative variables like sex,
visual acuity, IOP. Mean and standard deviation was computed for qualitative
variables like age and IOP. Chi square test was used to see the association of
pre and postoperative visual acuity and t-test was used to see mean ± standard deviation of pre and postoperative IOP.
RESULTS
Total
50 patients (28 male and 22 female) were included in the study. The age range
of patients was 41 – 74 with the mean 56.86 and standard deviation of 10.40.
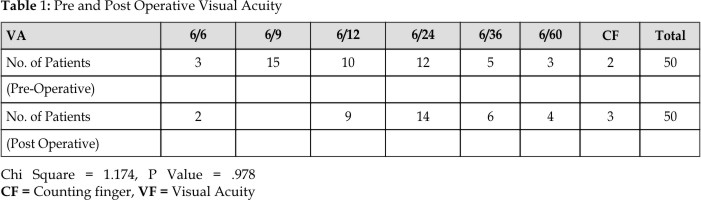
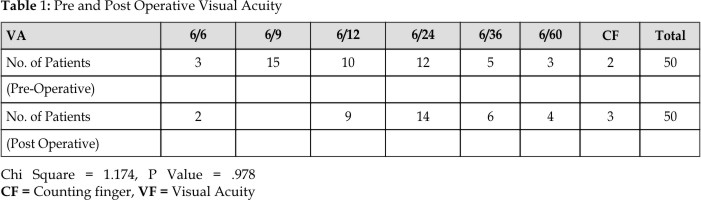
Table 1 shows the preoperative visual acuity and post operative best corrected
visual acuity after 1 year. These results indicate that there is no
statistically significant difference between pre and postoperative visual
acuity. In most of the patient’s visual acuity is maintained after 1 year of
surgery. The chi square is1.174 and P value is 0.978.
Preoperative
IOP was in the range of 20 – 55 mmHg, with the mean ± standard deviation of 32.70 ± 12.43.
Out of 50 patients, 10 (20%) had IOP in the range of 10 – 21 mmHg; 16 (32%) had
IOP in the range of 22-30 mmHg; 10 (20%) had IOP in the range of 31-40 mmHg; 10
(20%) had IOP in the range of 41 – 50 mmHg and 04 (08%) had IOP in the range of
51 – 55 mmHg. Postoperative IOP on 1st postoperative day was in the
range of 3-22 mmHg with mean ±
standard deviation of 11.20 ± 5.13.
Out of 50 patients, 06 (12%) patients had IOP < 05 mmHg; 25 (50%) patients
had IOP in the range of 8 – 10 mmHg; 10 (20%) had had IOP in the range of 11 – 16
mmHg; 09 (18%) patients had IOP in the range of 17 – 22 mmHg. Postoperatively
in 4 (8%) patients bleb was flat and digital massage was done. These 4 patients
were reviewed after 1 week. In 2 of these patients, IOP came to below 21 mmHg,
while other 2 needed beta blockers to bring the IOP below 21mmHg. These results
indicate that IOP is controlled in most of the patients that is statically
significant. P value is < .0001.

Range
of IOP at the 1st postoperative month was 3-20 mmHg. Out of 50
patients, 2 (4%) patients had IOP < 5 mmHg; 18 (36%) patients had IOP in the
range of
5 – 10 mm Hg; 20 (40%) patients had IOP in the range of 11 – 16 mmHg; 10 (20%)
patients had IOP in the range of 16 – 20 mmHg. Range of IOP in the 3rd
postoperative month was 5-18 mmHg. Out of 50 patients, 5 (10%) patients had IOP
in the range of 5 – 10 mmHg; 15 (30%) patients had IOP in the range of 11 – 12
mmHg; 25 (50%) patients had IOP in the range of 13 – 16 mmHg; 5 (10%) patients
had IOP in the range of 16 – 18 mmHg. Range of IOP in the 6th
postoperative month was 5-20 mmHg. Out of 50 patients, 5 (10%) patients had IOP
in the range of 5 – 10 mmHg; 15 (30%) patients had IOP in the range of 11 – 14
mmHg; 25 (50%) patients had IOP in the range of 15 – 18 mmHg; 5 (10%) patients
had IOP > 18 mmHg.
The
range of IOP in 12th postoperative month was 5-22 mmHg as shown in
table 2 with mean and standard deviation of 15.78 ± 3.71. Out of 50 patients, 5 (10%) patients had IOP in the range
of 5 – 10 mmHg; 25 (50%) patients had IOP in the range of 11 – 17 mmHg; 15
(30%) patients had IOP in the range of 18 – 20 mmHg and 5 (10%) patients had
IOP in the range of 21 – 22 mmHg; out of last 5 patients, 2 stopped using beta
blockers and 3 had cystic bleb. These results indicate that IOP is controlled
in 45 patients out of 50, that is statically significant. P value is < 0.0001.
Visual
fields and C/D ratio showed no significant change after 1 year of surgery.
Postoperative compli-cations were Hypotony in 5 (10%) patients Flat anterior
chamber in 6 (12%) patients due to bleb leak in 2 (4%) patients and excessive
drainage in 4 (8%) patients. All of them were managed with topical
cycloplegics, double patching and
aggressive anti inflammation Hyphema occurred in 10 (20%) patients,
lasted for 1 – 4 days and settled with conservative management. In our study
the mean IOP was 15.78 after 1 year of surgery. IOP controlled and visual
acuity maintained in 45 out of 50 patients. So in our study 90% cases achieved
target pressure after conventional trabeculectomy.
DISCUSSION
Glaucoma
affects between 60 and 70 million people worldwide and is the leading cause of
irreversible blindness.8 The aim of glaucoma therapy is to preserve
the visual function by achieving a “Target Pressure” in each patient. The so
called Target Pressure goal should actually be a range with an upper IOP limit
that is likely to reduce further damage to the optic nerve in a given patient.
The target pressure range needs to be reassessed or changed as comparison of
IOP fluctuations, optic nerve changes and / or visual field progression
dictate. In points with advanced glaucoma or normal tension glaucoma, the need
for especially low pressures should be recognized.9
We feel
that the aim of trabeculectomy is a constant maintenance of reduced IOP in
order to prevent further damage to visual function with the main goal to
improve or at least preserve the patient’s quality of life10. Studies
of trabeculectomy as initial therapy for glaucoma, however suggest that there
may be some advantages such as reduction of patient visits to the doctor and
possibly better visual field preservation.11 Surgery once had a bad
reputation because of high complication rates both at the time of operation and
later. The introduction of improved surgical instruments and suture material
has led to various refinements of original operation12. Since the
late 1960’s the operation of choice in POAG has been Trabeculctomy” in which
controlled fistula is created between the anterior chamber and the
subconjunctival space utilizing a partial thickness scleral trap door guarding
an internal sclerostomy.13
In
Britain and much of Europe, filtration surgery is performed early in the course
of the disease, without extensive use of medication.14 Advocates of
early surgery points to its high rate of success when performed early in the
course of the disease.15
A long
term multi center, prospective follow up study in Scotland, which compared
early trabeculectomy and conventional medical therapy, showed better IOP
control in the early surgery group, with less visual fields decay.15
In this study we have tried to find out whether the conventional trabeculectomy
will work in our population or not. All the cases in our study were diagnosed
case of POAG. We included the patients with the age ranging from 41 – 74 years.
All the patients were Pakistani belonging to different localities and different
postoperative behaviors. It was ensured that all patients were undergoing
trabeculectomy by the same skilled surgery. In the Moorfields Primary Treatment
Study16 the group of patients successfully treated by trabeculec-tomy
achieved a mean IOP of 14.5 mmHg,
compared with 18.5mmHg for the patients successfully treated with laser or
medication. The significantly lower IOPS in the surgical patients
were maintained throughout the initial 5 years follow up period. There was a
markedly high success rate of 98% (in terms of IOP control) in the surgical
group at 5 years, compared with 80% in the medical group and only 60% in the
laser patients. So our results are comparable to Moorefield’s Primary Treatment
Study.7,16 The difference is that they also observed the result of
laser and medication treatment.
Our
results are also comparable to that Baber et al.17 In their study,
out of 46 eyes, the IOP was maintained at below 21 mmHg without medication in 42
eyes (91.3%). The difference is that his study includes all types of primary
glaucoma. In our study the mean IOP is around 15 mmHg after one year of
surgery. IOP is controlled and visual acuity maintained in 45 out of 50
patients. So in our study 90% cases achieved success. In a nutshell although
convention a trabeculec-tomy is affective in controlling IOP in our population,
the obvious down side of any short term, small study is its limitation, but it
does present a trend, obviously in order to really prove whether conventional
trabeculectomy will be working long term, it requires longer set of patient and
a longer duration of study.
CONCLUSION
In our study the mean IOP is
15.78 after 1 year of surgery. IOP is controlled and visual acuity is
maintained in 45 out of 50 patients. So in our study 90% cases achieved success
after conventional trabeculectomy. Conventional trabeculectomy can be effective
in controlling intraocular pressure in patients with primary open angle
glaucoma in our population in the short term.
Author’s Affiliation
Dr. Ghazala Tabassum
Liaquat National Hospital
Stadium Road, Postal Code74800
Karachi
Dr. Imran Ghayoor
Liaquat National Hospital
Stadium Road, Postal Code74800
Karachi
Dr. Riaz Ahmed
Liaquat National Hospital
Stadium Road, Postal Code74800
Karachi
REFERENCES
1.
Yanoff and Ducker Ophthalmology.
Glaucoma: epidemiology of Glaucoma. 3rd edition. 2009; 10:
1095-1101.
2.
Quigley
HA, Broman AT. The number of people with glaucoma
worldwide in 2010 and 2020. Br J Ophthalmol. 2006; 90: 262-7.
3.
Gupta
N, Weinreb RN. New definition of glaucoma. Curr Opin
Ophthalmol. 1997; 8: 38-41.
4.
Dielemans I,
Vingerling JR,
Algra D,
Hofman A,
Grobbee DE,
de Jong PT. Primary
open angle glaucoma, intraocular pressure, & systemic blood pressure in
general elderly population: the Rotterdam Study. Ophthalmology. 1995; 102:
54-60.
5.
Higginbotham
EJ. Medication in the treatment of choice for
chronic open angle glaucoma. Arch Ophtalmol. 1999; 116: 239-40.
6.
Jampel
HD. Laser trabeculoplasty is the treatment of
choice of chronic open angle glaucoma. Arch Ophthalmol. 1998; 116: 240-1.
7.
Migdel
C, Gregory W, Hitchings RA. Long term functional outcome after
early sugery compared with laser and medicine in open angle glaucoma.
Ophthalmology. 1994; 101: 1651-7.
8.
Thylefors
B, Negral AD, Pararajasegaram R, Dadzie KY. Global
date on blindness. Bull World Health Org. 1995; 73: 115-21.
9.
Jampel
HD. Target pressure in glaucoma therapy. J
Glaucoma. 1997; 6: 133-8.
10.
Jagdish Bhatia Outcome of
Trabeculectomy Surgery in Primary Open Angle Glaucoma
11.
12.
Vernon
SA, Spencer AF. Intraocular pressure control following
microtrabeculectomy. Eye 1995; 9: 299-303.
13.
Waston
PG, Grierson I. The place of trabeculectomy in the
treatment of glaucoma. Ophthalmology. 1981; 88: 175-96.
14.
Jay
JL. Rational choice of therapy in primary open
angle glaucoma. Eye 1992; 6: 243-7.
15.
Jay
JL, Allen D. The benefit of early trabeculectomy versus
conventional management in primary open angle glaucoma relative to severity of
the disease. Eye 1989; 3: 528-35.
16.
Migdal
C, Hitchings R. Control of chronic simple glaucoma with
primary medical, surgical and laser treatment. Trans ophthalmol soc
17.
Baber
TF. An audit of 81 cases of trabeculectomies
in primary glaucoma in NWFP. Journal of Medical Sciences. 2000; 10: 37.